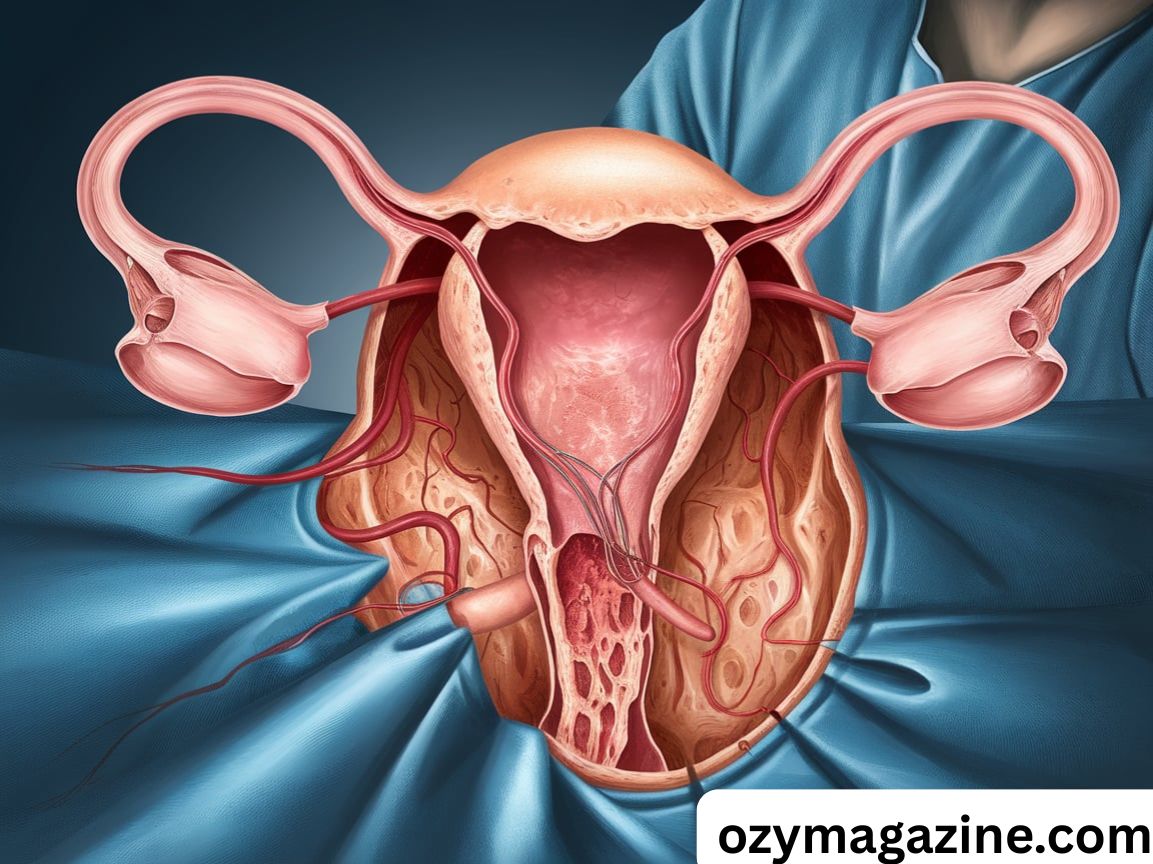
A partial hysterectomy is a surgery to remove the upper part of the uterus while keeping the cervix. It is also called a supracervical hysterectomy. This procedure helps treat problems like fibroids, bleeding, or endometriosis.
Living with heavy bleeding or constant pain can be hard. Many women try treatments that don’t work. A partial hysterectomy can bring real and lasting relief.
Doctors use different surgical methods like laparoscopic, abdominal, or vaginal hysterectomy. Recovery is usually quicker than with full hysterectomy. Many women feel better and return to daily life faster.
Key Takeaways
A partial hysterectomy removes only the top part of the uterus but keeps the cervix in place. This helps maintain the vaginal canal structure and can improve sexual function after hysterectomy. It is often chosen to treat issues such as chronic pelvic pain, heavy bleeding, or non-cancerous uterine growths.
The recovery time post-surgery can vary depending on the surgical technique used. Options like abdominal hysterectomy, laparoscopic hysterectomy, or vaginal hysterectomy affect how quickly you heal and how much discomfort you might experience.
This procedure also comes with long-term effects such as hormonal changes, especially if the ovaries are removed. After surgery, women may consider hormone replacement therapy (HRT) or non-hormonal treatments to manage menopause symptoms.
Partial Hysterectomy: A Surgery That Brings Relief
Many women suffer from gynecological health problems that don’t respond well to medications or non-surgical options. When symptoms like chronic pelvic pain, severe periods, or pain during sex affect your daily life, a partial hysterectomy can bring long-term relief.
In this type of gynecological surgery, the doctor removes only the upper uterus, leaving the cervix intact. This can help maintain better pelvic organ support, preserve nerve endings, and allow some women to feel more “whole” after the surgery. For others, it’s about avoiding bladder issues post-surgery and keeping natural function in place.
Women often choose a supracervical hysterectomy when their condition isn’t cancer-related. Keeping the cervix also means that Pap smears after hysterectomy are still needed, as there’s still a small risk of cervical cancer.
Procedure Overview
A partial hysterectomy is a type of uterus removal surgery that leaves the cervix in place. This method is considered when doctors believe that cervix preservation offers better outcomes for the patient’s physical and emotional health.
The surgery is performed using different surgical techniques, which may include:
- A large cut in the abdomen (abdominal hysterectomy)
- Small cuts and cameras (laparoscopic hysterectomy)
- Through the vagina (vaginal hysterectomy)
This decision depends on your medical history, body type, and the condition being treated. For example, large uterine fibroids may need open surgery, while smaller growths can be removed using minimally invasive surgery.
Conditions Treated
Many conditions of the female reproductive system can be treated with a partial hysterectomy, especially when they don’t respond to medications or lifestyle changes.
Uterine fibroids are the most common reason. These are non-cancerous uterine growths that cause heavy bleeding, pain, and pressure.
Endometriosis is another. This condition happens when tissue similar to the uterine lining grows outside the uterus. It leads to pain, infertility, and long periods.
Adenomyosis causes the uterine lining to grow into the muscle wall of the uterus, leading to pain, cramping, and bloating.
All of these problems can deeply affect a woman’s quality of life, especially when they cause pelvic pain and fatigue.
Comparing Types of Hysterectomies
Understanding the differences between total vs. radical hysterectomy and partial hysterectomy is important when planning your surgery. Each type removes different parts of the reproductive system and affects your hormonal balance differently.
Comparison Table: Types of Hysterectomy
| Type | What’s Removed? | Common Reasons | Pregnancy Possible? |
| Partial Hysterectomy | Upper uterus only | Fibroids, Endometriosis, Adenomyosis | No |
| Total Hysterectomy | Entire uterus + cervix | Cancer, Prolapse, Chronic bleeding | No |
| Radical Hysterectomy | Uterus, cervix, vagina (upper part), tissues, lymph nodes | Cervical cancer | No |
Total Hysterectomy
In a total hysterectomy, both the uterus and cervix are removed. This type of surgery is often used to treat more serious issues like uterine cancer, severe adenomyosis, or prolapse.
Because the cervix is removed, you won’t need Pap smears after hysterectomy, but this also changes the structure of the vagina, which can affect sexual function.
Radical Hysterectomy
This is the most extreme option. A radical hysterectomy removes the uterus, cervix, upper vagina, and surrounding pelvic tissues. It is usually only done when there is a high risk of cancer, especially cervical cancer.
Because so much tissue is removed, women who have this procedure may enter early menopause, especially if ovaries removal is also done. The emotional and physical recovery is more intense compared to a partial hysterectomy.
Surgical Techniques for Partial Hysterectomy
There are three main surgical techniques used in a supracervical hysterectomy. Your doctor will choose the best one for you based on your health, the size of your uterus, and whether you’ve had past surgeries.
Abdominal Hysterectomy
This is the traditional method. A cut is made in the belly to access the uterus. It’s often used when the uterus is large or when there are complications.
Healing takes longer, and there will be a visible scar. The recovery time post-surgery is usually around six weeks.
Laparoscopic Hysterectomy
This minimally invasive surgery uses a tiny camera and tools inserted through small cuts. It allows for faster recovery, less bleeding, and less pain.
This is often the best method for women who want a quicker hysterectomy recovery and who have smaller fibroids or uterine lining conditions.
Vaginal Hysterectomy
In this surgery, the uterus is removed through the vagina. There are no visible scars, and post-surgery care is usually easier. But this method may not be possible for women with a large uterus or scar tissue.
It’s also considered safer in terms of avoiding hysterectomy complications, but it requires a very experienced surgeon.
Risks and Complications
Like any major surgery, a partial hysterectomy carries risks. These may include bleeding, infections, nerve damage, or injury to nearby organs like the bladder or bowel.
Other complications may involve vaginal prolapse, bladder issues post-surgery, and reactions to anesthesia. Women with conditions like diabetes or obesity may face higher risk.
Always talk to your doctor about the hysterectomy risks and benefits before deciding.
Long-term Effects

Over time, a partial hysterectomy can bring both relief and changes. Keeping your cervix may help with sexual function and reduce your chances of pelvic organ shifting.
If your ovaries are removed, you’ll experience hormonal changes similar to menopause. This can lead to bone loss, hot flashes, mood swings, and heart disease risk.
That’s why hormonal balance and proper post-surgery care are critical for long-term health.
Post-Surgery Recovery
Healing after a partial hysterectomy depends on the type of surgery you had. Most women take between 2 to 6 weeks to recover fully.
You should avoid sex, heavy lifting, and strenuous exercise during this time. Always follow your surgeon’s advice and attend all check-ups.
Hospital Stay and Initial Recovery
Most women stay in the hospital for 1 to 3 days. Pain is usually managed with medication. You’ll be encouraged to walk around slowly to prevent blood clots.
Avoid putting anything in the vagina, including tampons or douches, for at least 8 weeks to prevent infection.
At-Home Care and Follow-Up
At home, you’ll need rest, hydration, and proper nutrition. Slowly increase your activity and avoid lifting anything heavy. Many women return to work in about 4 weeks, depending on the surgery type.
Follow-up visits are crucial to track healing, manage any hormonal changes, and monitor for hysterectomy complications.
Hormone Treatment Options After Hysterectomy
If your ovaries are removed, your body will stop producing estrogen and progesterone, which causes sudden menopause symptoms. Hormone therapy may be recommended to restore hormonal balance.
Hormone Replacement Therapy (HRT)
HRT helps relieve hot flashes, night sweats, and mood swings. It also protects against bone loss and supports your heart. If you still have your uterus, a mix of estrogen therapy and progestin therapy may be used. If only your ovaries are gone, estrogen alone may be enough.
Non-Hormonal Treatments
Some women prefer to avoid hormones due to the risk of breast cancer or liver disease. In this case, lifestyle changes such as diet, exercise, and medications like SSRIs or gabapentin can help manage menopause symptoms.
Read Also : How Alcohol Before and After Surgery Can Impact Your Recovery
Making an Informed Choice About Partial Hysterectomy
Choosing a partial hysterectomy is a big decision. It’s not just about the surgery, but also about your long-term health, hormones, and emotional well-being.
Always speak openly with your doctor, ask questions, and understand all your options. Whether you’re facing endometriosis, fibroids, or adenomyosis, knowing the facts helps you take control of your gynecological health and choose the path that brings relief and healing.
Understanding the Emotional Impact of Partial Hysterectomy
A partial hysterectomy doesn’t just affect your body—it also has emotional and psychological effects. Many women feel a mix of relief, sadness, and anxiety after the procedure, especially when it comes to fertility or body image.
Support from family, friends, and therapists can make a big difference. Understanding that emotional healing is part of post-surgery care helps women feel more empowered and less alone.
How Cervix Preservation Affects Life After Surgery

Keeping the cervix intact helps preserve the natural vaginal canal structure, which can benefit sexual satisfaction and reduce recovery time. Many women report better outcomes in terms of comfort and emotional well-being.
However, cervix preservation still requires regular Pap smears after hysterectomy. Staying on top of screenings ensures continued protection against cervical cancer and other health concerns.
Exercise and Nutrition Tips for Faster Recovery
Light walking and gentle stretching can help improve circulation and speed up hysterectomy recovery. Always start slow and follow your doctor’s advice to avoid complications like internal bleeding or strain.
Eating iron-rich foods, drinking plenty of water, and avoiding processed meals supports healing and reduces fatigue. Good nutrition also supports hormonal balance after uterus removal.
FAQ,s
What are the benefits of a partial hysterectomy?
A partial hysterectomy relieves symptoms like heavy bleeding and pelvic pain while preserving the cervix, which may support better sexual function and quicker recovery.
What happens to a woman after a partial hysterectomy?
After a partial hysterectomy, periods stop, but hormones may remain stable if the ovaries are left, and regular Pap smears are still needed.
What is the difference between a partial and a full hysterectomy?
A partial hysterectomy removes only the upper uterus, keeping the cervix, while a full hysterectomy removes both the uterus and cervix.
What happens when the ovaries are left after a hysterectomy?
If the ovaries are kept, natural hormone production continues, reducing the risk of early menopause and helping maintain hormonal balance.
Conclusion
A partial hysterectomy is more than just a medical procedure—it’s a step toward reclaiming comfort, confidence, and control over your gynecological health. Whether you’re dealing with chronic pelvic pain, uterine fibroids, endometriosis, or adenomyosis, this surgery offers real relief when other treatments haven’t worked.
With the right surgical technique, proper post-surgery care, and support through hormonal changes, most women go on to live healthy, active, and fulfilling lives. Choosing this path can feel overwhelming at first, but being informed makes all the difference. Talk openly with your healthcare provider, understand your options, and take charge of your healing journey. You’re not just removing pain—you’re making room for a better quality of life.